Maldives: Ending TB in Five Years (Case Study)
- June 26, 2021
- Evelyn Lee
- Posted in education
Maldives: Ending TB in five years

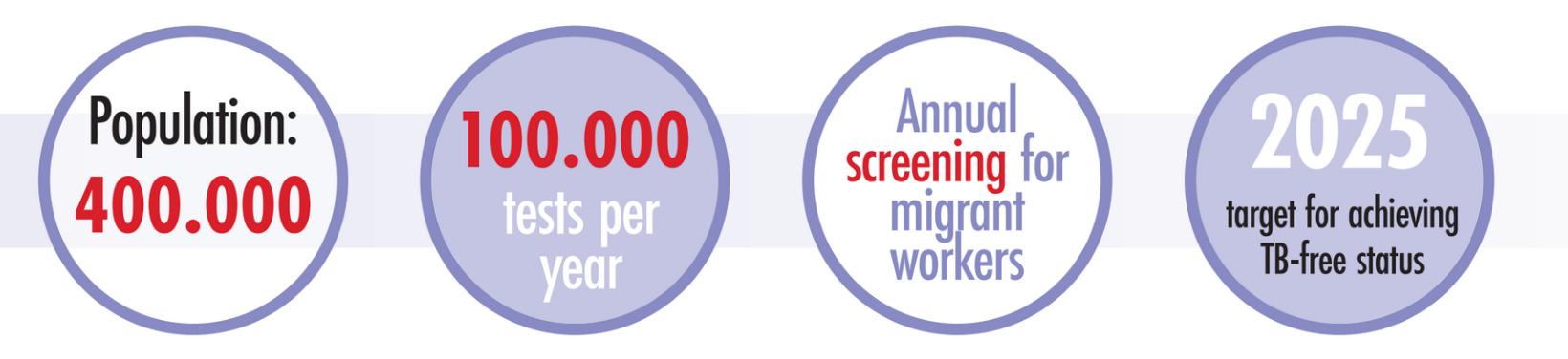
The Maldives has set itself the ambitious goal of gaining TB-free status by 2025. To achieve this, detecting and treating cases of latent TB infection (LTBI) is crucial. Over the next five years, doctors will carry out an estimated 100,000 tests per year, both on migrant workers from high-TB countries and the local population, screening for LTBI.
Dr Mohamed Ismail is a respiratory physician at the Indira Gandhi Memorial Hospital in Malé and the chair of the Maldives’ technical advisory group on TB. In these roles he advises on all matters relating to TB in the country and acts as the clinical focal point for the national TB programme. In this case study, Dr Ismail discusses the rollout of Oxford Immunotec’s T-SPOT.TB test as part of nationwide, systematic population screening to eradicate TB in the country and prevent future outbreaks.
Focus on the Maldives
The Maldives has long been at the forefront of TB control in South Asia. With a small population of around 400.000 spread across 26 atolls, outbreaks of TB are more effectively controlled than in many other countries in the region. Since the 1970s, the country has also run a successful programme for TB control, which includes BCG vaccination, screening, diagnosis and treatment. As a result, the incidence of TB in the late 1990s was reduced to only a handful of cases.
Since then, increased tourism in the Maldives and immigration from countries with a high burden of TB have led to an increase in the number of cases and has made TB a renewed public health concern. Dr Ismail says: “In recent years, we are doing more work in diagnosing, especially sputum negative tuberculosis. We have been using the GeneXpert® molecular test for the last three years and we will start doing TB culture later this year. However, the national strategic plan is to eliminate TB completely, so we are now aiming to become a TB-free country by 2025. This is the main target of the national TB programme.”
Focus on LTBI
Key to achieving TB-free status will be detection and treatment of LTBI. This latent form of TB is common in many countries in the region, but because people can carry LTBI for many years without showing symptoms of the disease, detection can be challenging. Dr Ismail explains: “It is impossible to know if and when these cases will become active, but they act as a reservoir for active TB and unless we treat them, we cannot reduce our TB burden. We currently use the Mantoux test as and when needed, but this test requires two visits and suffers from low reliability. Moving forward we want to follow WHO guidelines for tackling LTBI, which recommend the use of interferon-gamma release assays (IGRAs) for screening.”
IGRAs are sensitive blood tests that can detect LTBI within 24 hours. Unlike the Mantoux test, IGRAs only require a single patient visit and the result of the test is not affected by previous BCG vaccinations.
For the T-SPOT.TB test, a single blood sample is collected into a single standard tube. From this sample, peripheral blood mononuclear cells (PBMCs) are isolated. A specific number of PBMCs is then used for detecting the interferon gamma released in response to MTB-specific antigen stimulation. This ensures reliability regardless of a person’s immune status. A substrate is then added that visualises a spot at every location where an interferon-gamma-releasing T cell was positioned, providing easy, visual assessment of the result. This method creates a normalised IGRA, which is key to reducing the variability often seen in other test methods. This approach to LTBI screening avoids treatment delays, is suitable for use in vulnerable patients and reduces unnecessary treatments, which can cause side effects such as hepatotoxicity.
Choosing the T-SPOT.TB test
When choosing an IGRA to be used as part of the nationwide TB programme, it was essential to take local infrastructure characteristics into account. Although every atoll in the Maldives has a hospital, the resources that are available in each hospital vary. For this reason, it was important that sample collection was as simple as possible so that each hospital could carry out collection and send the samples elsewhere for analysis.
Commenting on choosing the T-SPOT.TB test, Dr Ismail says: “It has excellent sensitivity and its easy sample collection makes it well suited for a country like the Maldives. In some of the peripheral islands we do not always have well-trained laboratory staff, so we have to transport the samples to larger centres. With the T-SPOT.TB test, sample collection is easier and more convenient, leading to fewer errors due to sample handling.”
“The other important aspect,” Dr Ismail continues, “is the performance of the T-SPOT.TB test in the immunosuppressed population and in children, where it is better and more sensitive than other IGRAs. LTBI is more common in these groups and it is also more likely to develop into active TB compared to the general population, so reliable detection in these groups is vital.”
With the T-SPOT.TB test, sample collection is easier and more convenient, leading to fewer errors due to sample handling
~ Dr Mohamed Ismail
~ Dr Mohamed Ismail
Looking ahead
From March 2020, doctors at the Indira Gandhi Memorial Hospital are planning to screen an estimated 100,000 people per year. Over the coming years, the entire local population will be offered screening and there will be annual testing for migrant workers from high-risk countries. As part of this process, more hospitals in other atolls will be equipped with test analysis capabilities in order to reduce transport time and therefore overall time-to-result. Using the T-SPOT.TB test will ensure reliable detection of LTBI, even in groups that are hard to screen, which means the Maldives are on track to achieve TB-free status in 2025.